ANALYSIS: Coronavirus in Africa - to mask or not to mask, that is the question
SUMMARY
|
With the globe in the grips of coronavirus fever, African countries suddenly find themselves among the affected nations. By 11 March there were 98 confirmed cases across the continent, in nine countries. Naturally, interest in ways to prevent infection has been increasing exponentially.
Retail stores have battled to keep up with panic buying of hand sanitisers, while demand for protective masks is brisk - if you can get your hands on one at all.
But are these face masks effective? Who should use them? We take a closer look at what reliable research shows.
What is coronavirus?
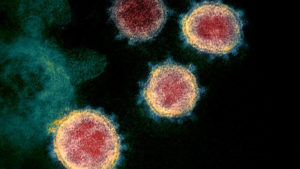 This image shows the spikes on the outer edge of the SARS-CoV-2 particles that give coronaviruses their name, 'corona' or crown-like. Photo: NIAID-RML/Flickr" />
This image shows the spikes on the outer edge of the SARS-CoV-2 particles that give coronaviruses their name, 'corona' or crown-like. Photo: NIAID-RML/Flickr" />According to the World Health Organization, coronaviruses are a large family of viruses that can cause illness in animals and people.
When viewed under a powerful microscope, coronaviruses look like a halo or a “crown” - “corona” in Latin.
In people they cause illness ranging from the common cold to previous global scares such as Middle East respiratory syndrome-related coronavirus (Mers) and severe acute respiratory syndrome coronavirus (Sars).
The current global concern is around the most recently discovered coronavirus, which causes the coronavirus disease 2019, abbreviated as Covid-19.
The virus that causes it has been officially named severe acute respiratory syndrome coronavirus 2, or Sars-CoV-2.
How is the coronavirus spread?
Our current knowledge of how Covid-19 spreads is based largely on what we know about other types of coronavirus. The coronavirus attaches itself to cells in the small air sacs in our lungs. It invades the cell, hijacks the biochemical machinery inside, and begins making copies of itself. When an infected person sneezes or coughs, these copies are expelled from the body inside microscopic drops of mucus.
The viral copies can find their way onto the skin of people nearby or the surface of objects such as clothing, railings or cell phones. The virus can be transferred from objects to hands, and from hands onto objects.
Reports show that depending on the type of surface it lands on and the external temperature, Sars-CoV-2 can remain infectious for two hours to up to nine days.
If we then touch our faces, it's only a short hop via an air current into our noses or mouths and, eventually, lungs. These types of spread are known as droplet and contact spread respectively.
Surgical masks, eye protection, gowns and gloves are considered appropriate personal protective equipment when caring for an infected patient. But what about when you’re just trying to go about your daily business and want to avoid getting infected?
Face masks more effective on infected patients

Cloth masks are popular in Asia, but some other parts of the world may be more familiar with two different types of mask: surgical or medical face masks and N95 respirators.
Medical face masks, loose-fitting rectangles that cover the nose and mouth, are used by operating theatre staff during procedures. They were initially designed to protect the patient from coughed or exhaled secretions by doctors, nurses and other healthcare workers during sterile procedures. More recently, research is beginning to reveal that they may also protect the healthcare worker.
Studies have shown that despite their lack of seal and loose fit, surgical masks can indeed trap germs. In a study published in 2016, researchers at Stony Brook University Hospital in New York built a closed chamber model using two mannequin heads, one acting as an infectious source and the other as a receiver. Particles of radioactive dust were used as a stand-in for viruses. The dust was spread by simulated “coughs”.
They found that putting a face mask on the infectious mannequin was more effective in reducing the final amount of inhaled dust than putting either a face mask or N95 respirator on the receiving mannequin.
Scaled up to the real world, a 2015 review by Australia’s University of New South Wales of studies on face masks’ effectiveness in preventing infection identified two that tested the exhaled air from people with influenza. When face masks were used, there was a more than threefold reduction of viral particles in exhaled samples.
What about N95 respirators?

N95 respirators, on the other hand, are the go-to protective device when medical workers are trying to avoid contact with respiratory pathogens. In South Africa, clinical staff are familiar with the respirators because of the protection they give against tuberculosis.
The secret to their function is in the name. “N95” isn’t a brand name, it’s a filtration standard. The “95” in N95 refers to filter efficiency. Tested against aerosol droplets 0.3 micrometres in diameter (about 200 times finer than the tip of a human hair), they must be able to filter 95% of particles this size or larger. They filter much smaller particles with comparable efficiency.
The coronavirus is about 0.1 micrometres in diameter, but because it is spread in microscopic droplets, which are a lot larger (more than 5 micrometres), they comfortably fall into the filtration range.
How does the research on respirators translate into practice? A review of 23 laboratory studies from 1998 to 2014 by researchers in Canada found that N95 respirators filter viruses as well as can be expected, given compliance standards.
But there’s one important drawback to using N95 masks. Leaks from the gaps in poorly fitted N95 masks allowed 14% to 40% of viral particles to escape filtration during inhalation. This finding also applied to surgical face masks.
How do N95 respirators hold up in the real world?
In 2011 the Cochrane organisation reviewed 67 studies that used various forms of protection, from handwashing to respiratory measures, in hospitals.
They found that for respiratory viruses, N95 respirators reduced people’s chances of becoming ill by about six times when compared to the people in the study who didn’t use them. Surgical masks cut the odds to about a third, and handwashing to half.
Done and dusted? Not really. A 2016 review of studies in the Canadian Medical Association Journal found that N95 respirators appeared to only have a protective advantage over surgical masks in laboratory settings.
But the data did not show that N95 respirators were better than surgical masks in protecting health care workers against transmissible respiratory infections in a clinical setting. Other large studies, published nearly 10 years apart, have also been inconclusive. N95 respirators, it seems, are only more effective than face masks in specific conditions.
For healthcare workers, the take home message is that there are many factors, not just inhalation, in the transmission of viruses such as the coronavirus. By catching the largest droplets and preventing facial contact, even the humble face mask helps reduce infection.
But what about ‘out there’ in communities?
What about local communities, where people may not be trained in how to put on and take off face masks, and dispose of them properly?
Frustratingly, the data isn’t nearly as strong - but here’s what we know so far.
In 2009 a team from the University of New South Wales investigated if face masks could prevent sickness in family members caring for sick children. They recruited 286 adults from 143 households where a child had recently been diagnosed with a respiratory illness.
They found that both face masks and N95 respirators reduced the daily risk of infection by 60% to 80%. (The researchers do urge caution in applying this figure to any other context.)
In 2015 the same team reviewed nine studies where face masks were analysed in a community setting in a preventative method, worn by healthy participants. They found that while there was a small decrease in the number of illness episodes, the size of this wasn’t large enough to be distinguishable from random chance.
A standout effect was that when face masks were combined with handwashing there was an even larger, cumulative preventive benefit, especially in the early phases of disease outbreaks.
What does begin to emerge from the research is that handwashing also has a noticeable effect on respiratory virus transmission, even larger than face masks in some studies. Face masks and handwashing used together as an early precaution have an even larger impact.
Bottom line? Wash your hands!
This isn’t the first time Africa Check has advocated for the simple intervention of washing hands. In our 2017 piece on whether Vitamin C can prevent a common cold, where respiratory viruses where once again on the chopping block, we did the same.
We have found three meta reviews on handwashing, conducted by different institutions in different years. They reveal that handwashing can reduce the risk of contracting respiratory illness by anything from 6% to 48% in individual studies, with a reported average reduction of about 20%.
‘Incredibly inefficient’ for everyone to wear masks
How long should masks be worn? The Centers for Disease Control recommends that surgical masks be disposed of after every encounter with a patient. For respirators it says the same should "ideally" also apply, but also if they become deformed or damaged, visibly dirty, no longer form an effective seal to the face, wet or come into contact with bodily fluids.
And as infection numbers climb, we need to be efficient with our resource spending on a global scale to ensure there’s enough to go around. The safest solution would be for everyone to wear masks, wash their hands, wear protective clothing and avoid close contact. But this is incredibly inefficient.
More practical evidence-based recommendations are:
- Handwashing is effective and easy. Everyone should regularly wash their hands.
- Surgical face masks are generally effective, but most effective when worn by sick people and by people caring for the sick.
- N95 respirators should only be used by people trained to do so, and only show a distinct benefit over face masks in specific circumstances.
These recommendations are supported by the public positions of the US Centers for Disease Control, the World Health Organization and, most recently, the Journal of the American Medical Association.
Petrie Jansen van Vuuren is a medical doctor based in Gauteng, with a postgraduate background in human physiology research at the University of Pretoria.




Add new comment