The lifestyle sections and health pages of many major newspapers and magazines routinely tout questionable health claims that are not supported by scientific research or evidence.
Some, like a dietician’s advice to eat eggplant to stave off colon cancer, may seem relatively harmless. Others can have severe repercussions. Take for instance the many treatments being falsely peddled as cures for HIV. If patients forsake their proven-to-work antiretroviral treatment in favour of these “cures”, the outcome will most certainly be devastating.
Given that false health claims are often perpetuated by people who, at first glance, appear to be credible professionals, it is not always clear that the treatments they are touting are unproven. We have put together this guide to assist journalists, editors and Joe Public in telling fib from fact.
Says who?
 When testing the legitimacy of health claims it pays to embrace your inner sceptic. Do not take anything at face value. Instead, ask: “Who has made this claim, what are their credentials and can those credentials be independently verified?”
When testing the legitimacy of health claims it pays to embrace your inner sceptic. Do not take anything at face value. Instead, ask: “Who has made this claim, what are their credentials and can those credentials be independently verified?”Be aware, for instance, that titles can be deceiving. “Doctor” can refer to any number of things: a medical doctor (MD), a doctor of philosophy (PhD), a doctor of science (ScD), an honorary doctorate or even a sham “doctorate” purchased online from one of the many websites that peddle bogus qualifications.
To get to the bottom of this, do a quick search for the credentials and associations of the person or organisation making the claim. Are their qualifications relevant to their claims? For example, the founder of this natural therapy centre boasts an impressive list of accolades, among them a doctorate in philosophy. He does not, however, mention having a medical degree, despite offering treatment for a range of clinical conditions including TB and cancer.
The consumer website CAMcheck.org features an interesting exercise in picking apart what appear to be false claims made in an alternative health practitioner’s resume.
Check and check again
 Be wary if you cannot independently verify someone’s academic qualifications. Similarly, be cautious of companies and organisations that claim to be legitimate but have a limited footprint on the web.
Be wary if you cannot independently verify someone’s academic qualifications. Similarly, be cautious of companies and organisations that claim to be legitimate but have a limited footprint on the web.Usually companies and organisations have a clearly marked and detailed “about” section on their website and often also list their board of directors there. That is a good place to start. Who are the directors? Are they really on the board of the organisation or company? What are their qualifications and backgrounds and can those qualifications be verified independently?
Take for example the manufacturers of this product which is reported to make people with HIV well. If you visit their website you will quickly discover that they are suspiciously opaque about who they are and what they do. It stands to reason that anyone looking to market a proven treatment would be embracing publicity, not shying away from it.
Often just having a look to see who else is talking about a claim can help you discern between fact and fiction. Important breakthroughs in medicine will be covered by major news agencies, websites, radio stations and television channels and published on reputable medical websites. If the treatment has not received recognition in these channels, it is unlikely that there is sound evidence that it works.
The devil is in the detail
 Sometimes it is the smaller stuff that gives away a false health claim. Inconsistencies, half-truths and disclaimers are all hints that the product or its promoter might not be sincere. Is it clear what the ingredients of the treatment are, what its mechanisms of action are and how effective it is?
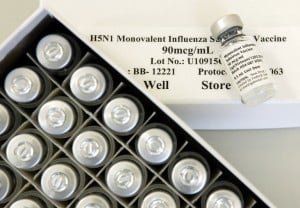
Sometimes it is the smaller stuff that gives away a false health claim. Inconsistencies, half-truths and disclaimers are all hints that the product or its promoter might not be sincere. Is it clear what the ingredients of the treatment are, what its mechanisms of action are and how effective it is?This product, though packaged to look like medicine and accompanied by a double-helix with the heading “Preserve your DNA”, claims it is “not a pharmaceutical product or medicine”. Then why try to look like one?
False claims are often supported by anecdotal evidence and personal testimonies that make a product seem very effective. But without scientific proof that a treatment works, these endorsements are about as reliable as office gossip.
To determine whether a treatment is safe and effective, it must undergo an extensive protocol of clinical testing where it is first deemed safe for human consumption and is then given to a large sample of people to determine whether it is effective. In order to obtain conclusive proof that the treatment works, it is compared to a placebo. This is known as a “controlled trial”.
Clinical trials and patient safety
 Not all of this research is published, although there is growing support for this information to be made universally accessible. The abstracts of most published studies are available online and they should give you a good overview of the findings. Google Scholar will bring up results from most reputable academic journals. The Medline database also features a comprehensive collection of published research.
Not all of this research is published, although there is growing support for this information to be made universally accessible. The abstracts of most published studies are available online and they should give you a good overview of the findings. Google Scholar will bring up results from most reputable academic journals. The Medline database also features a comprehensive collection of published research.Whilst there are arguments that the clinical trial process is prohibitively expensive for less profitable treatments, trials are considered integral to ensuring patient safety.
If you were unable to find any published research to support a claim, approach the person or organisation marketing the product or service and ask what evidence they can provide for the effectiveness of their product.
Remember: If a treatment has not been tested on humans, it cannot be considered safe or effective. If the study was not controlled and the sample was not large enough, the findings cannot be considered conclusive. (Later phases of clinical testing involve thousands of participants).
You might be told the product has been tested or is currently being tested, but without the results of these tests, the claim remains unproven. Wherever possible, also speak to a reputable expert in the relevant field to get their views on the issue and to help you make sense of complicated research.
Keep in mind that just because there is no conclusive proof that a treatment works, it does not necessarily mean it isn't effective. It simply means it has not (yet) been subjected to rigorous testing. In that case, saying with certainty that a treatment does not work would be incorrect.
However, selling or otherwise promoting a treatment or cure without proof that it does work is deeply unethical and should be called into question. It usually also means not enough is known about the safety of a particular treatment. It is important that these concerns are raised and readers are made aware of the lack of evidence and the repercussions this may have for them.
First, do no harm...
 Sometimes patients will still choose to take a treatment even if they know there is not yet conclusive proof that it works. Their decision may be influenced by cultural norms or a need for spiritual engagement. Traditional herbal practitioners are often consulted as counsellors and spiritual healers, not just for the treatment of physical ailments.
Sometimes patients will still choose to take a treatment even if they know there is not yet conclusive proof that it works. Their decision may be influenced by cultural norms or a need for spiritual engagement. Traditional herbal practitioners are often consulted as counsellors and spiritual healers, not just for the treatment of physical ailments.Others may be inherently sceptical of modern, allopathic medicine and choose to look for what they consider more natural treatment options. Often this is spurred on by the common misconception that because something is labelled “herbal” it cannot be harmful. This belief is easily challenged by the fact that technically, nightshade, oleander and hemlock are all herbal, though definitely not safe for human consumption.
Interestingly, the placebo effect suggests that even if treatments are proven to have no effect at all, they may still have some positive impact on the people taking them simply because they believe it will make them feel better.
All these considerations make it extremely important that even if treatment is known to be ineffective, it is at least safe for human consumption. And if it is not, the public has a right to be told this in no uncertain terms.
In some cases those promoting a treatment will offer guidelines for safety. The Placenta Network, for instance, is clear about the precautions that need to be taken when new mothers decide to consume their placenta, a practice they say will assist in recovery after birth.
In other cases the safety of supposed treatment can be less clear and you may have to consult a medical doctor to get a better sense of the risks involved. Some herbal treatments can induce vomiting and thus interfere with the effectiveness of existing medication. There is research suggesting the African potato, once championed as a potential anti-HIV treatment, may actually be harmful to people living with HIV.
Follow the money
 Some health claims are more dubious than others. Here it helps to follow the money. Sometimes false claims can be the result of misinterpreted or insufficient research, intended to inform or entertain. We see examples of this where a certain food is singled out for its beneficial properties without sound evidence to back up the claim.
Some health claims are more dubious than others. Here it helps to follow the money. Sometimes false claims can be the result of misinterpreted or insufficient research, intended to inform or entertain. We see examples of this where a certain food is singled out for its beneficial properties without sound evidence to back up the claim.In one case examined by Africa Check, an article suggested dates can cure stomach cancer. We found no evidence to support this claim, only a study in which an extract derived from dates shrank tumours in mice. This is a far cry from having proof that eating dates is a treatment for stomach cancer.
Claims like these should be interrogated, particularly because they come at the cost of more moderate and valid advice like paying attention to diet overall to stave off lifestyle disease. But other claims can be far more extortionate and are deserving of very serious scrutiny.
Herbal treatments can sell for large sums of money. Convincing the desperate and hopeful to part with their scant funds without actual proof that these treatments work constitutes fraud and should be exposed as such.
Do not assume regulators keep the sale of quack cures in check
 As consumers, we easily fall into the trap of thinking all treatments being sold in reputable pharmacies or on legitimate-looking websites have been tested and proven effective. But it would be a mistake to assume that the government or any regulating body can weed out all false claims or that the public is protected from quack cures because their sales are not legal.
As consumers, we easily fall into the trap of thinking all treatments being sold in reputable pharmacies or on legitimate-looking websites have been tested and proven effective. But it would be a mistake to assume that the government or any regulating body can weed out all false claims or that the public is protected from quack cures because their sales are not legal.In South Africa the Medicines Control Council has boards for regulating African traditional medicines and complimentary and alternative medicines. Neither have succeeded in effectively controlling the sales of unproven remedies. Although, change seems to be afoot with the drafting of a new regulation that once implemented, will require all alternative medicines making health claims to register with the Medicines Controls Council. Whilst the new measures will clamp down on quality and safety of products, depending on the condition the product claims to treat, it will be less strict on requiring proof that the treatment actually works. The new regulations do not apply to African traditional medicine.
Whilst proven treatments are usually marketed directly to the medical community, quacks often go straight to the media and rely on the press to advertise their products to the public. This makes it critically important that reporters take the time to interrogate health claims before publishing them.
It is not always possible, practical or fair to label a treatment as ineffective or to make out a salesman as a fraud. But unless there is conclusive evidence that they are effective and safe, health claims should always be presented as what they are: merely claims.


Add new comment